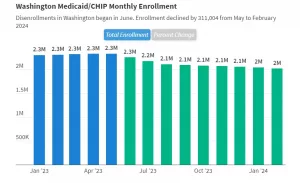
LEWISTON, ID—As of March 26th, nearly 19.2 million Medicaid enrollees had been disenrolled based on the most current data from all 50 states and the District of Columbia. Starting April 2023, states were allowed to start removing people from Medicaid after a three-year federal pause on removals—due to the COVID-19 pandemic—ended.
Overall, 31% of people with a completed renewal were disenrolled in reporting states, while 69%, or 40.6 million enrollees, had their coverage renewed. Due to varying lags for when states report data, the data reported undercount the actual number of disenrollments to date.
In Idaho, approximately 185,000 people lost health insurance coverage on Medicaid, which insures people with disabilities or who are considered low-income. The state opted for a six-month timeline for resuming Medicaid eligibility reviews, which are known as Medicaid unwinding.
Idaho’s process began in April, and as of December, nearly 130,000 enrollees renewed their coverage, and 156,000 were disenrolled, including nearly 43,000 determined ineligible and more than 113,000 disenrolled for procedural reasons.
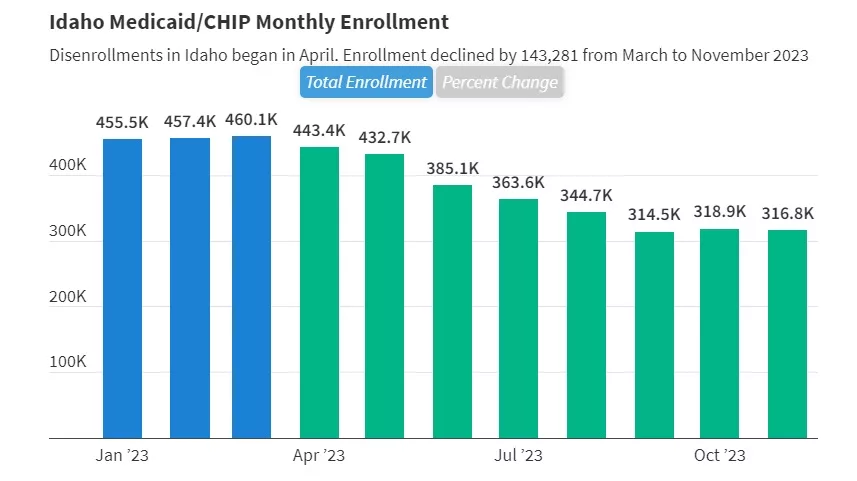
Disenrollments in Washington began last June. Enrollment declined by 311,004 from May to February 2024.
As of February, just over one million enrollees renewed their coverage, and nearly 433,000 were disenrolled, including 64,000 who were determined ineligible and 368,000 who were disenrolled for procedural reasons.
For more information, visit the KFF Medicaid and Unwinding Tracker.